Last Updated on June 22, 2022
Introduction
Birth control (oral contraceptives) is considered the first-line treatment choice for endometriosis flare-ups. If you’ve been diagnosed with endometriosis or are suffering from one or more symptoms linked to this painful condition, such as dysmenorrhea (painful periods), pain during intercourse, or pain during bowel movements or urination, these medicines can help with pain management.
The symptoms may greatly affect the quality of life, and symptom control should be the primary aim of initial management. Contraceptive pills provide symptom relief and can cause an improvement in physical, mental, and social well-being.
Have a read to learn more about Endometriosis, its symptoms, and management, whether birth control for endometriosis is the right choice and Endometriosis vs. PCOS.
What is Endometriosis?
It’s a chronic inflammatory disorder, that happens when tissue similar to the uterine lining, called endometrium, grows outside of your uterus. This includes the ovaries, fallopian tubes, and outer surfaces of your intestines. This tissue bleeds like the tissue in your uterus.
It can also form endometriosis flare-ups, which can cause inflammation and scarring. Endometriosis affects an estimated 5.5 million women in North America and 176 million women worldwide.
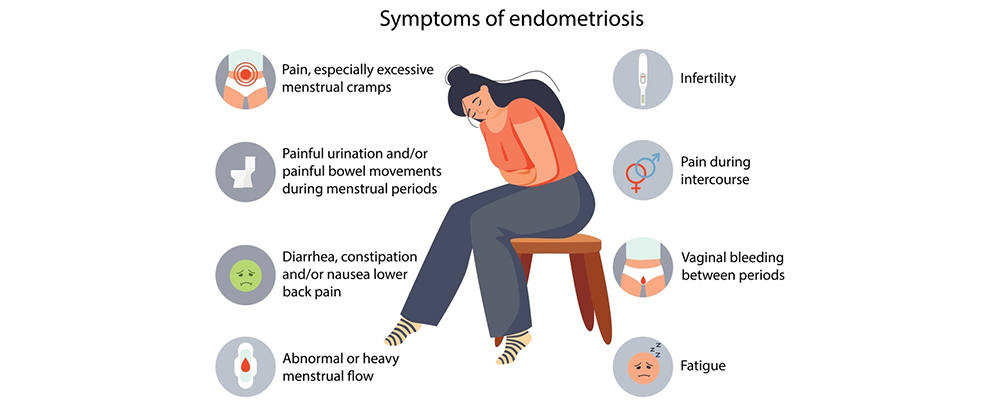
Some common symptoms of endometriosis include:
Painful periods (dysmenorrhea):
Pelvic pain and cramps can start before a menstrual period and last for several days. you may also have lower back and abdominal pain.
Pain with intercourse:
With endometriosis, pain during or after sex is common.
Pain with bowel movements or urination:
You will probably experience these symptoms during a menstrual period.
Excessive bleeding:
You might experience intermenstrual bleeding, i.e., occasional heavy menstrual periods or bleeding between periods. A few times, endometriosis has been first diagnosed in those seeking infertility treatment.
Other signs and symptoms:
During menstrual periods, you may have fatigue, diarrhea, constipation, bloating, or nausea.
The seriousness of the pain may not be a reliable indicator of the degree of your condition. You could have mild endometriosis with a lot of pain or advanced endometriosis with very little pain. Endometriosis is often mistaken for other conditions due to its symptoms of pelvic pain, such as pelvic inflammatory disease (PID) or ovarian cysts. It might also be confused with irritable bowel syndrome (IBS), a condition that causes bouts of diarrhea, constipation, and abdominal cramping. If anytime IBS accompanies endometriosis, this can complicate the diagnosis and hence the treatment.
What Causes Endometriosis?
While the specific cause of endometriosis is uncertain, there have been several possibilities proposed:
- Genetics – individuals are more likely to experience endometriosis flare-ups if their family members have the disorder.
- Retrograde menstruation – occurs when some of the womb linings flow up through the fallopian tubes and embed themselves in the organs of the pelvis.
- Immune system complications – the immune system serves as the body’s natural defense against disease; when it’s interrupted, the disease is more likely to occur.
- Endometrial cell movement – endometrium cells can spread through the bloodstream and lymphatic system.
Endometriosis is a typical gynecological condition. It is estimated that it affects 6 to 10% of women of childbearing age and is a significant reason for pain and infertility. Endometriosis’ physical symptoms can be controlled but not healed. Symptoms of endometriosis often last till menopause. Many women may wonder, “Does Birth Control Help With Cramps?”
Birth control for endometriosis is one of the most popular methods in the United States to treat this debilitating condition. It is believed that it can ease the pain and might decrease the growth of lesions.
How is Endometriosis Diagnosed?
Your doctor will ask you to describe your symptoms, including the location of your pain and when it happens, to diagnose endometriosis and other disorders that can cause pelvic discomfort. Tests to check endometriosis are:
Pelvic Examination:
Your doctor manually palpates areas of your pelvis for abnormalities such as cysts on your reproductive organs or scars behind your uterus. Small regions of endometriosis are often difficult to detect unless they have caused a cyst to form.
Ultrasound:
This test creates images of the inside of your body using high-frequency sound waves. A transducer is either pushed against your abdomen or put into your vaginal canal to acquire the images (transvaginal ultrasound). To gain the best image of the reproductive organs, both forms of ultrasound might be used. Although a routine ultrasound imaging test won’t tell your doctor if you have endometriosis, it can detect cysts associated with the disease (endometriomas).
Laparoscopy:
Your doctor may send you to a surgeon for an operation that permits the physician to see into your abdomen (laparoscopy). Your surgeon creates a tiny incision near your navel and inserts slander viewing equipment (laparoscope) to examine for evidence of endometrial tissue outside the uterus while you’re under general anesthesia.
The location, extent, and size of endometrial implants can all be determined using a laparoscopy. A tissue sample (biopsy) may be taken by your surgeon for further testing. Your surgeon may be able to treat endometriosis during the laparoscopy with correct surgical planning, resulting in only one procedure.
Is Endometriosis Curable?
While endometriosis may not go away completely, it can be managed with a variety of treatments, including
Anti-inflammatory medications and NSAIDs (i.e. ibuprofen):
To reduce uncomfortable menstrual cramps or endometriosis flare-ups, your doctor may prescribe an over-the-counter pain medicine such as ibuprofen (Advil, Motrin IB, and others) or naproxen sodium (Aleve).
Hormone therapy:
Endometriosis discomfort can be reduced or eliminated with the use of supplemental hormones. Endometrial implants thicken, break down, and bleed when hormone levels rise and fall during the menstrual cycle. Hormone therapy may help to reduce endometrial tissue growth and prevent new endometrial tissue implants.
Hormonal birth control:
Birth control pills, patches, and vaginal rings help regulate the hormones that cause endometrial tissue to develop each month. Many women notice lighter and shorter menstrual flow when using hormonal contraception. In some circumstances, using hormonal contraceptives — particularly continuous-cycle regimens — can help to minimize or eliminate pain.
Medications that release gonadotropin hormone (GnRH) agonists:
These medications stop ovarian-stimulating hormones from being produced, reducing estrogen levels and preventing menstruation. As a result of this endometrial tissue shrinks.
Surgery (i.e. hysterectomy):
The uterus can be removed (hysterectomy) to address signs and symptoms of endometriosis, such as excessive monthly bleeding and painful menses due to uterine cramping, in persons who don’t want to become pregnant.
Doctors typically prescribe less intense treatments to start with. If none of these treatments work, surgery may be suggested as a final resort.
How do Birth Control Pills Treat Endometriosis?
Birth control medications reduce the production of hormones that regulate ovulation and menstruation, which helps with endometriosis. This may help control endometriosis flare-ups in several ways:
- Making periods lighter and shorter
- Reducing endometrial-like tissue development outside the uterus
- Reducing inflammation related to the menstrual cycle
- Altering one’s perception of pain
Endometriosis oral contraceptives prevent the menstrual cycle from functioning normally. A woman usually ovulates halfway through her period. The uterine lining grows and expands after that. It breaks down if a person does not become pregnant.
Oral contraceptives can prevent ovulation by stopping the hormones that induce it from fluctuating. It will not be able to eradicate existing lesions or endometriosis flare-ups, but it may be able to prevent the formation of new ones.
Which Birth Control Pill is Best for Endometriosis?
Typically, estrogen-progesterone pills are the most beneficial, but progesterone-only pills can also be helpful. Progesterone-only pills were praised for their effectiveness in treating endometriosis-related pelvic pain. Some researchers have noted that both norethindrone acetate and dienogest — progesterone-only oral contraceptives — may be a better option when compared to combined estrogen-progesterone birth control pills. Taking birth control medicines may help with your pain levels, but you may experience some side effects like mood swings, headaches, or tender breasts, depending on the type of birth control you take.
Birth control pills shouldn’t be taken if you have:
- Blood clots, a history of blood clots, a blood clotting disorder (Factor V Leiden, for example)
- Coronary artery disease
- History of stroke or heart attack
- Cancer (i.e., breast cancer, cancer of the uterus, cervix, or vagina)
- Unusual or unexplained vaginal bleeding
- Suspected pregnancy
- Lupus
- History of smoking
How long does Hormonal Birth Control Take to Work?
According to the National Institute for Health and Care Excellence, it takes 3–6 months for people to notice if birth control for endometriosis is a helpful treatment. People may, however, begin to notice changes before this time.
A doctor can offer different medications if birth control isn’t helpful to relieve endometriosis symptoms.
Does Birth Control Help With Cramps?
Birth control helps cramps. These pills make periods lighter and shorter (or even stop them completely while you’re on birth control). However, they are less dependable; some people experience more irregular periods when using these approaches. However, they’re still extremely useful for relieving period cramps.
Endometriosis vs. PCOS (Polycystic Ovary Syndrome)
Endometriosis and polycystic ovary syndrome are diseases that affect women of reproductive age who have vaginal tissue. This includes people between the ages of 12 to 52. Both of these disorders produce menstrual irregularities, which can result in severe bleeding. They can also make it more difficult to conceive.
The other symptoms are different, however. They also involve different hormonal issues. Excess estrogen, a feminine hormone, is connected to endometriosis. Excess androgens, or male hormones, are the cause of PCOS. It’s also conceivable to have both of these circumstances at the same moment.
As a result, the disorders produce a variety of symptoms and necessitate a variety of treatments. Let’s read the difference between endometriosis vs. PCOS.
Endometriosis vs. PCOS
|
High amounts of androgen hormones, which are male sex hormones, are caused by polycystic ovarian syndrome (PCOS). Hormonal birth control is one of the therapy options for both PCOS and endometriosis, therefore a person may discover that it helps with both conditions.
However, some types of birth control can increase androgen levels, which may not be helpful for people with PCOS. A doctor may recommend non-androgenic combination contraception or a progesterone-only alternative.
Bottomline
For many women with endometriosis, hormonal birth control can be a successful treatment. Although it will not cure the problem, it will help to prevent new lesions from forming, relieve pain, and regulate the menstrual cycle.
There is no one-size-fits-all solution that will work for everyone, so a person may need to test a few different types before settling on one. If birth control for endometriosis does not seem to work, doctors can advise you on additional treatment options.




