Last Updated on February 20, 2023
Difference between Crohn’s and Colitis – Overview:
Have you been suffering from stomach cramps for weeks? Do you feel exhausted and have gained weight? And you’re always running to the restroom. What exactly is going on? Possibly you have inflammatory bowel disease (IBD) — Crohn’s and Colitis. Which one, though?
Two of the most common inflammatory bowel diseases are Crohn’s disease and ulcerative colitis (UC). IBD affects approximately 1.6 million Americans, with 70,000 new cases diagnosed each year. IBD can be diagnosed at any age, but it is more common in patients between the ages of 15 and 30. It also affects up to 80,000 children in the United States. IBD equally affects both men and women.
Crohn’s and colitis share many characteristics, including long-term inflammation in the digestive system. However, there are some significant differences that affect treatment. Multiple Clinical Research Organizations like ours are conducting Crohn’s disease and Ulcerative Colitis research studies to help find these potential treatments and further understand these conditions.
Similarities between Ulcerative Colitis and Crohn’s Disease:
Although the diseases can occur at any age, they are most common in teenagers and young adults. Men and women are equally affected by Crohn’s and Colitis.
Symptoms of Crohn’s and colitis:
Crohn’s disease vs. Ulcerative colitis: These conditions have very similar symptoms. Both UC and Crohn’s disease have unknown causes, and both have similar types of contributing factors such as environmental, genetic, and abnormal responses by the body’s immune system.
Distinctions between Ulcerative Colitis and Crohn’s Disease:
Crohn’s disease vs. Ulcerative colitis – There are three significant distinctions:
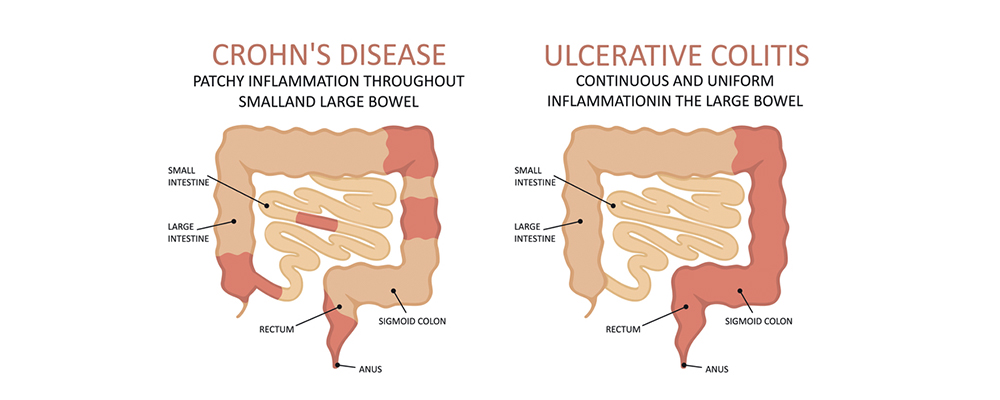
1. The location:
Only the large intestine is affected by ulcerative colitis. However, Crohn’s disease can cause inflammation anywhere in the digestive tract.
2. Ongoing inflammation:
Crohn’s disease patients frequently have healthy areas in between inflamed areas. There are no healthy areas between inflamed spots in ulcerative colitis.
3. The layer affected:
Because Crohn’s disease affects more of the GI tract, it can cause issues that doctors rarely see in patients with ulcerative colitis. As an example:
Sores in the mouth between the gums and the lower lip, or on the sides or bottom of the tongue. Anal tears (fissures), ulcers, infections, or narrowing are all possibilities.
Now, Look at the Difference between Crohn’s and Colitis:
Overview of Crohn’s Disease:
Crohn’s disease can cause inflammation in any part of the body, from the mouth to the anus. However, the disease most commonly affects the junction of the small intestine and the colon (ileum). Crohn’s disease affects equally to both men and women. Although the disease affects patients of all ethnicities, research indicates that it is more common among the Eastern European Jewish population.
Crohn’s Disease Subtypes:
Crohn’s disease is classified into five types:
- Crohn’s colitis: This affects only the colon.
- Gastroduodenal Crohn’s disease: It is a chronic inflammation of the stomach and the first part of the small intestine, or the duodenum.
- Ileitis: This affects just the ileum.
- Ileocolitis: This is the most common form of Crohn’s disease, affecting the ileum and colon.
- Jejunoileitis: The disease affects the upper half of the small intestine, known as jejunoileitis.
Crohn’s Disease Symptoms:
Crohn’s disease symptoms include diarrhea that lasts more than 6 weeks, abdominal pain, and weight loss. Blood and mucus in the stool are present in up to 50% of Crohn’s disease patients.
Crohn’s Disease Causes:
The specific cause of Crohn’s disease is unknown. Scientific research, on the other hand, has identified three risk factors for Crohn’s disease.
The three elements are as follows:
- Smoking or a history of smoking increases a person’s risk of developing Crohn’s disease.
- Genetics: Those with Crohn’s disease in their immediate family are more likely to develop it.
- Mucosal immune system: The immune system initiates an inflammatory response against “normal” bacteria in the digestive tract.
Overview of Ulcerative Colitis:
Ulcerative colitis is a chronic inflammation of the large intestine or colon that is one of the two main types of inflammatory bowel disease (IBD). In ulcerative colitis, the inflammation begins in the rectum and spreads throughout the colon.
Ulcerative Colitis Types:
Ulcerative colitis is classified into several types based on the area of the colon affected.
- Ulcerative proctitis is an inflammation that only affects the rectum. Ulcerative proctitis is typically a milder form of UC due to the limited area of the diseased bowel.
- The rectum and sigmoid colon are both affected by proctosigmoiditis.
- Left-sided ulcerative colitis: In this type of ulcerative colitis, the inflammation begins in the rectum and progresses to the splenic flexure.
- Pancolitis affects the entire colon.
Ulcerative Colitis Symptoms:
The colon cannot absorb water from the materials that pass through it because of inflammation and ulceration in the intestine lining. This causes a variety of ulcerative colitis symptoms, including:
- Diarrhea
- Abdominal pain
- Bowel urgency
- blood in the stool.
- Anorexia
- Weight loss
Outside of the intestine, ulcerative colitis can cause a variety of symptoms in other parts of the body, including:
- Itchiness, redness, and pain around the eyes
- Mouth sores
- Swelling in joints
- Rashes and sores on the skin
- Osteoporosis
- Stones in the kidney
Ulcerative Colitis Causes:
The specific cause of ulcerative colitis is unknown. Medical research has identified three major factors that contribute to the development of ulcerative colitis, including:
- Inflammatory Response
- Environmental
- Genetics
How Do You Obtain the Correct Diagnosis of Crohn’s and Ulcerative colitis?
Because the differences between the two conditions Crohn’s and colitis mostly revolve around where inflammation occurs in the digestive system, the best way for a doctor to give a correct diagnosis of IBD is to look inside.
You may be given tests such as:
- X-rays can reveal areas of your intestine that are blocked or unusually narrow.
- Contrast X-rays, which require you to swallow a thick, chalky barium liquid in order for doctors to see how it moves through your system.
- CT scans and MRIs are used to rule out other conditions that may cause symptoms similar to IBD.
- Endoscopy is a procedure in which a doctor looks inside your digestive system with a tiny camera attached to a thin tube. Endoscopies of various types can:
- Examine the lower section of your large intestine. This test is known as a “sigmoidoscopy” by your doctor.
- Examine the length of your large intestine. A colonoscopy is being performed.
- Examine the esophageal, stomach, and duodenum linings. It is an EGD (esophagogastroduodenoscopy).
- Additional testing with a pill-sized camera to examine your small intestine. This is also known as pill or capsule endoscopy.
- The bile ducts in the liver and the pancreatic duct are two examples. This is referred to as ERCP (endoscopic retrograde cholangiopancreatography).
Scientists are working to improve several blood tests that aid in the diagnosis of Crohn’s and colitis. They look at the levels of certain antibodies in the blood. Two examples are:
- “pANCA” (perinuclear anti-neutrophil antibodies)
- “ASCA” (anti-Saccharomyces Cerevisiae antibody)
People with ulcerative colitis frequently have the pANCA antibody in their blood, while those with Crohn’s disease have ASCA. However, for the time being, the tests have questionable accuracy and should only be used in conjunction with the above testing.
Even after all of these tests, doctors may be unable to determine which of the two conditions you have. That is true for one out of every ten people with IBD. They exhibit symptoms of both diseases. Because it is unclear which disease they have, they are given the diagnosis of “indeterminate colitis.”
What are the Complications of Crohn’s disease vs. Ulcerative colitis?
People with Crohn’s or colitis are more likely to develop conditions that occur outside of your gastrointestinal tract (also known as ‘extraintestinal manifestations’), such as anemia, mouth sores, Osteoporosis, skin conditions, liver conditions, and cancer are all examples of diseases that can affect your eyes or joints. Fistulas and abscesses, adhesions, structure, anal fissures, and hemorrhoids are all gastrointestinal conditions associated with IBD.
Complications can cause troubling symptoms such as constipation, pain, fatigue, and weight loss. They can also impair your ability to perform daily activities such as work and school, as well as engage in personal and social activities.
ANXIETY AND DEPRESSION:
People who have Crohn’s disease or colitis are more likely to suffer from anxiety and depression. Anxiety and depression can have a negative impact on a person’s quality of life, interfering with their ability to perform daily activities such as work and school, and increasing their risk of disability.
Anxiety and depression are associated with a history of surgery, disease complications, cigarette smoking, and being female in people with IBD. Major depression (clinical depression) is a type of depression that is so severe and persistent that it interferes with daily functioning.
ANAL FISSURES:
Anal fissures are small tears or sores in the anus lining. When you pass stool, they can cause sharp pain and bleeding. Anal fissures are common in Crohn’s disease but uncommon in ulcerative colitis. Anal fissures can appear even before other signs and symptoms appear.
HEMORRHOIDS:
Hemorrhoids are enlargements of the blood vessels around the anus. They can cause itchiness, soreness, or swelling around the anus, as well as pain and bleeding when passing stool.
OBSTRUCTION:
Obstruction (intestinal blockage) is a serious complication of IBD and a potential emergency. Obstruction may necessitate immediate surgery.
Obstruction usually affects the colon (large intestine) or the small intestine, especially if there are prior strictures or adhesions. Bloating, nausea and vomiting, and abdominal pain are all possible symptoms.
PAIN AND DISCOMFORT IN THE JOINT:
Arthralgia is another term for joint pain. Arthralgia affects roughly half of all IBD patients. In addition to joint pain, people suffering from arthralgia experience joint stiffness and swelling.
Arthralgia can occur in a variety of joints throughout the body, including the hands, knees, and ankles.
The symptoms of arthralgia are similar to those of arthritis. Arthritis, which means that a joint is not only painful but also inflamed, is also common in people with IBD. There is no joint inflammation in arthralgia.
ARTHRITIS:
Arthritis is characterized by joint inflammation and pain. Arthritis affects approximately 20% of Crohn’s disease patients and 10% of ulcerative colitis patients.
Arthritis that develops in IBD is not the same as rheumatoid arthritis. Rheumatoid arthritis is a type of arthritis that gradually destroys the joints. People with IBD arthritis have arthritis that does not destroy or degrade the joints.
MALNUTRITION:
Malnutrition, or a lack of proper nutrition, is a major issue with IBD. It is the primary cause of long-term weight loss. IBD patients are frequently underweight, with nutritional deficiencies as well as changes in body fat composition, muscle mass, and bone mineral density (which puts them at risk of fractures). They are generally tired and weak, with low energy.
Anemia, or a lack of red blood cells in the blood, can result from malnutrition. This can cause fatigue and other issues. Malnutrition also makes it difficult to recover from illness.
FISTULAS:
Fistulas are small tunnels that can form in your intestine. They can connect to other parts of the intestine, the skin, or other internal organs.
The rectum is responsible for more than half of all fistulas. A perianal fistula is the most common type of fistula, and it opens in the area around the anus. Fistulas can also connect the rectum or intestine to the skin, the bladder, or the vagina.
Fistulas can sometimes burrow to the skin or to a blind end, where fluid can accumulate. An abscess occurs when the fluid becomes infected. This is extremely painful, can cause a fever, and can spread to your bloodstream.
A Day in the Life of Someone with Crohn’s and Ulcerative Colitis:
Even though they must take medications, people with these conditions live useful and productive lives. When they are not experiencing a flare-up of their disease, they feel fine and are frequently symptom-free.
Despite the fact that there is no cure, medical therapy has improved the health and quality of life for the majority of people with Crohn’s and colitis. Current research may lead to further advancements in medical and surgical treatment, as well as a cure.
What is the Treatment for Crohn’s and Colitis?
The goal of treating these conditions is to make you feel better (induce remission), minimize medication side effects, and promote mucosal healing. This is the actual healing of your gut mucosa or lining. The purpose is to improve not only your symptoms, but also the health of your gut, and then maintain that improvement. Long-term health benefits from a healthier gut.
Crohn’s and Colitis Medications:
Because no two Crohn’s or colitis cases are alike, there is no “one-size-fits-all” approach to medication and treatment. The medications prescribed by your doctor, as well as the dosage and side effects you may experience, will be unique. When you are in remission or have a flare-up, you and your doctor must collaborate to determine the best treatment plan for you.
Antibiotics, sulfasalazine and 5-ASAs, immunosuppressants, steroids, biologics, and biosimilars are among the medications used to treat Crohn’s and colitis. When medications are no longer effective, your IBD specialist may recommend surgery. Emerging treatments such as Fecal Microbiota Therapy (FMT) may also provide the opportunity to participate in clinical trials under the supervision of a clinician.
The Takeaway:
Crohn’s disease and ulcerative colitis can coexist in the same individual. The rarity of such cases lends support to the idea that Crohn’s and colitis are distinct diseases rather than different manifestations of the same disease process.
While there is no cure for Crohn’s disease, medications and lifestyle changes can help keep the infection at bay and prevent complications. There are numerous Crohn’s disease paid clinical trials in Michigan that could help you and countless others suffering from this disease. Keeping to your treatment plan, living a healthy lifestyle, and avoiding triggers can all help you manage this condition.





