Last Updated on April 10, 2023
Introduction
About 8 out of 10 women must have had an HPV infection at some point in time by the age of 50. Therefore, there is an emerging need to be able to talk openly about high-risk HPV, and not feel ashamed, or reluctant to discuss a sexually transmitted virus. So, understanding whether or not is cervical cancer genetic, and an overview of risk factors capable of the development of cervical cancer is important for early intervention. In such circumstances, an HPV DNA test can help tear down the uncertainty of “Is cervical cancer genetic” or “an amalgamation of environmental and habitual influence.”
While your family and friends take care of your emotional and moral values, prioritizing your health is essential. To revolutionize patient care, Revive Research Institute is conducting HPV cervical cancer screening, investigating novel therapeutic approaches for women. Enrolling in clinical trials might help in the identification of cervical cancer abnormalities in the cervix.
This blog talks about whether or not is cervical cancer genetic, an overview of risk factors, causes of cervical cancer, and more.
HPV and Cervical Cancer
“Is cervical cancer genetic?”
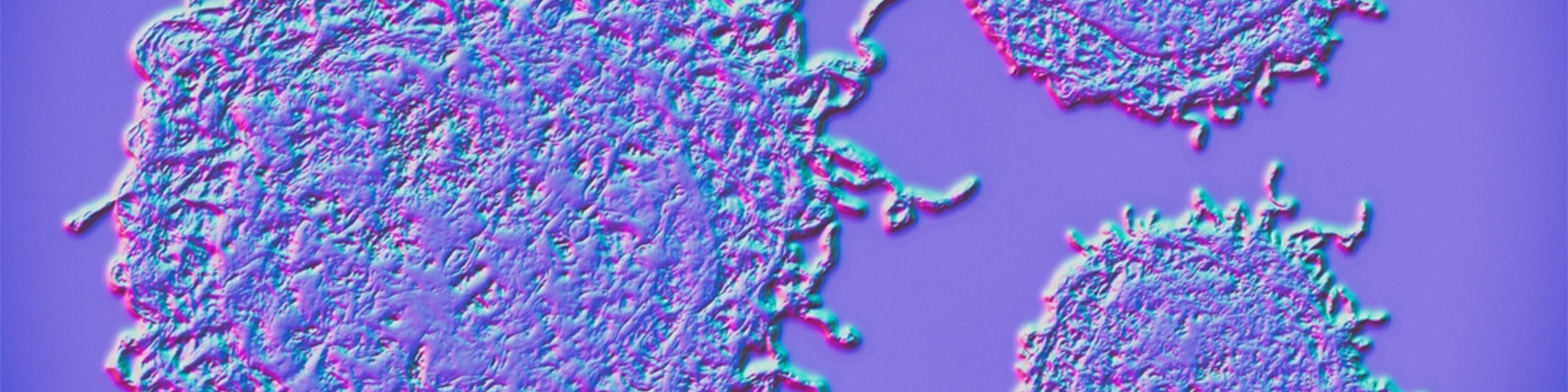
There is no simple answer to this. A correlation prevails between human papillomavirus (HPV) and cervical cancer. HPV is diagnosed as the most common cause of sexually transmitted diseases and cervical cancer.
The pathophysiology behind cervical cancer is the growth of abnormal cells lining the cervix and in the majority of cases is the result of HPV (95% cases). Additionally, the most commonly reported type of cervical cancer in most women is “squamous cell carcinoma”. Accounting for 70% of the cases.
Want to understand a bit more about Cervical Cancer and HPV Screening? Check out this informative piece on Let’s Talk Cervical Cancer and HPV Screenings.
Individuals Omitted from Cervical Cancer
Any woman, trans-man, or non-binary individual with a cervix is at risk of cervical cancer regardless of the causative factor. An exception to this is, those individuals who have undergone a total hysterectomy procedure (surgery done to remove the womb and cervix) are excluded from the risk of developing cervical cancer.
Is Cervical Cancer Genetic?
In spite of the fact that HPV infection can be contracted by anyone, keeping an eagle’s eye on early signs (not always evident) is important. This is because if the symptoms are not checked upon, they may evolve to cause cervical cancer.
Moreover, if you are someone with a family history of cervical cancer, you may be at a higher risk of developing the disease at some point in your life. Early detection is crucial for effective cervical cancer treatment, and scheduling routine gynecological visits and screening is essential for this purpose.
However; the answer to the question “ Is cervical cancer genetic?” is not always yes!
An overview of risk factors (which can be controlled) that possibly increase the vulnerability to cervical cancer are:
- Chalamadiya (bacterial) infection
- Immuno-compromised individuals, i.e HIV or AIDS
- Active birth cycle (more than 3 full-term pregnancies)
- Early pregnancy (<18 years)
- Active sexual life (sexually active, under 18 years of age, or have had multiple sexual partners)
- Smoking (women who smoke tobacco are twice likely at risk of developing cervical cancer)
An overview of risk factors, susceptible to inclination towards cervical cancer, but can not be seized are:
- Hormonal medicine diethylstilbestrol (DES) – prevents miscarriage
- History of vaginal, vulval, kidney, or bladder cancer
- Under 45 years – young people are more prone to getting cervical cancer
- Family history of cervical cancer
Causes of Cervical Cancer
“Is cervical cancer genetic?”
Genetics is a rare cause of cervical cancer. As stated previously, the origin of cervical cancer is the most infectious. Human papillomavirus (HPV) 16 and 18 (the most common viral infection of the reproductive tract) is a commonly identified culprit for most cervical cancers. In other cases, immunocompromised women (HIV infected) are 6 times more likely at risk of developing cervical cancer. Other non-infectious factors such as smoking tobacco products is a potential etiological factor for the onset of cervical cancer but is rarely addressed. Several studies have reported the presence of tobacco remnants in the cervical mucus of habitual smokers.
Signs of Cervical Cancer
Cancer is a silent form of the disease. It silently brews inside your body without manifesting signs of the disease in its early stages. Hence, in the earliest and most treatable stages, cervical cancer may not produce noticeable signs and symptoms. Instead, a pap test showing abnormal results may provide the first warning indication of precancerous or cancerous changes that might have occurred in the cervix. Usually, the symptoms advance slowly over several years before they eventually turn fatal.
The most commonly experienced symptoms are:
- Unusual vaginal bleeding after sex, in between periods, or after menopause
- Postmenopausal spotting or bleeding
- Increased vaginal discharge with sometimes a foul odor
As cervical cancer progresses, the severity of symptoms advances to:
- Persistent back, leg, or pelvic pain
- Loss of appetite and weight loss
- Vaginal discomfort
- Swelling of lower extremities
Diagnostic Approach
If cervical cancer is suspected, your gynecologist will likely perform a thorough clinical examination of your cervix for a definitive diagnosis. Colonoscopy is a procedure in which a special magnifying instrument (colposcope) is commonly used to look for any abnormal growths in the cervix.
On the other hand, a “Pap Test” is a reliable and relatively simple screening test or diagnostic test prescribed by doctors to confirm cervical cancer.
Preventive Measures
“Is cervical cancer genetic?” Answering this question, genetics should not be the only causative factor you would think of after reading this blog.
Remember, prevention is better than cure should be a mantra to live by. Merely, adapting to preventive measures can help revert some of the degenerative damage caused by HPV. These may include:
- Regular cervical screening for women between the ages of 25-64 years
- HPV vaccination for children between 12-13 years as a preventive measure against genital warts
- Condoms
- Intra-uterine device
- Eating a healthy and balanced diet
- Former smokers
- Limited sexual activity
Treatment Modalities
Certain factors such as your health status (comorbidities), stages of cervical cancer, and economic status (preferences) play a vital role in narrowing down the treatment of choice. A wide spectrum of available treatment options are:
- Cervical cancer surgery (hysterectomy, or trachelectomy)
- Radiotherapy
- Chemotherapy
- Immunotherapy
- Palliative care
Takeaway
Chronic infections (HPV, HIV, AIDS) if not discovered and timely eradicated expose women to a higher risk of developing cervical cancer. The importance of routine screening is that it allows early identification of the pre-cancerous lesions at stages where they can easily be treated. Therefore; understanding an overview of risk factors, and whether or not is cervical cancer genetic is important for every woman.