Last Updated on December 21, 2023
What is Crohn’s Disease?
Crohn’s disease, also called regional enteritis or ileitis is a type of inflammatory bowel disease (IBD) that causes inflammation of the gastrointestinal tract (GIT). It is an autoimmune-mediated inflammatory condition that can affect any part of the GI tract from the mouth to the anus. People suffering from Crohn’s encounter flare-ups like abdominal pain, diarrhea, weight loss, and often rectal bleeding.
Crohn’s can be distressing, painful, and draining and may sometimes lead to fatal complications. The disease primarily involves the intestinal system but can also affect kidneys, joints, bones, eyes, and liver.
It is believed that as many as 780,000 people in the United States have Crohn’s disease. While there’s no known remedy for Crohn’s disease medication can decrease Crohn’s disease flare-ups, and can help one achieve long-term recovery from the inflammation. With treatment, numerous people with Crohn’s disease can carry on with their routine life. Various Clinical Research Organizations in Michigan dedicated to conducting clinical trials to find a potential treatment for this disease.
Origin of Crohn’s Disease:
The root cause of Crohn’s disease is not yet confirmed. For a long time, diet and stress were thought to be causing Crohn’s. However, specialists today understand that these factors could worsen, but can’t be a cause for the Crohn’s disease flare-ups. A couple of factors like family history, a weak immune system, and environmental factors are involved in the occurrence of this disease.
Family history:
IBD (Irritable Bowel Disease) often runs in families. Individuals who have relatives suffering from Crohn’s are thought to be at higher risk of developing the disease. There are several specific mutations in the genes that can predispose one to develop Crohn’s disease. However, a lot of people with Crohn’s disease don’t have a family background.
Immune System:
Viral or bacterial infections are believed to be some of the causing factors of Crohn’s disease. Whenever your immune system attempts to fight back the attacking microorganism, an unusual response makes the immune system attack the cells in the gastrointestinal system.
Smoking:
Cigarette smoking could as much as double your risk of acquiring this fatal disease.
Crohn’s Disease Risk Factors:
- Heredity: People, who have any family member suffering from the same disease are at a higher risk, such as a parent, sibling, or child.
- Age: Crohn’s disease occurrence is not limited to any age, but you’re most likely to get this infection when you’re young. Most individuals who are above the age of 30 are diagnosed with Crohn’s.
- Race: Although Crohn’s disease can affect any racial group, Caucasians are at great risk, especially people of Eastern European (Ashkenazi) Jewish descent. Nevertheless, the incidence of Crohn’s has increased among African Americans who reside in North America and the United Kingdom.
- Cigarette smoking: Cigarette smoking is the most important yet controllable risk factor for developing Crohn’s disease. Smoking may help prevent ulcerative colitis. However, its harm to overall health outweighs any benefit, and quitting smoking can improve the general health of your digestive tract, as well as provide many other health benefits.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These include ibuprofen, naproxen sodium, diclofenac sodium, and many others. They can cause inflammation of the bowel which can aggravate Crohn’s disease flare-ups.
Crohn’s Disease Symptoms:
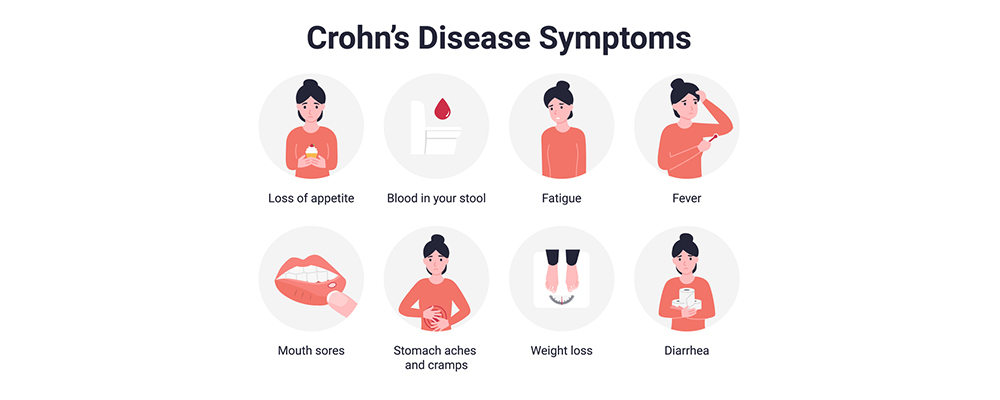
Crohn’s disease symptoms can go from mild to severe. For the most part, they grow step by step. But at times, Crohn’s exacerbates out of nowhere, abruptly. However, there will be times when you have no sign of any flare-up (remission).
One common question a lot of people ask is, “Is Crohn’s disease fatal?” This gastrointestinal condition can influence any part of the GI tract, from the mouth to the anus. While Crohn’s disease symptoms vary from one person to another, there are certain flares of irritation of the gut brought about by the condition that may be fatal. The flares could have symptoms such as:
- Persistent Diarrhea,
- Strong urge to move bowels,
- Stomach issues and pain,
- A sensation of incomplete bowel evacuation,
- Constipation, which can prompt bowel obstruction,
- Reduced appetite and weight loss, and
- Mouth sores.
At times such symptoms are mistaken with those of another condition, for example, food poisoning, an upset stomach, or an allergy. You should see your physician if any of these symptoms persist for a more extended period.
The symptoms worsen as the condition progresses. Severe Crohn’s disease includes symptoms like:
- Inflammation of skin, eyes, and joints,
- A perianal fistula, which causes pain and drainage around your anus,
- Kidney stones,
- Rectal bleeding,
- Inflammation of the liver or bile ducts,
- Shortness of breath and decreased ability to exercise due to iron deficiency (anemia), and
- Delayed growth or sexual turn of events, in youngsters.
Is Crohn’s Disease Fatal?
Crohn’s disease is not usually fatal, but it can lead to certain complications that can be life-threatening. It is a long-term inflammatory bowel disease (IBD), that most commonly affects the ileum, which is the end section of the small intestine, and the first section of the large intestine, or colon.
Depending on the location and severity of the disease, a person with Crohn’s may develop serious complications.
In this article, we have identified some life-threatening complications of Crohn’s disease and described its associated symptoms. Being aware of these complications, a person can talk to a doctor as soon as possible. Prompt treatment can increase the likelihood of a good recovery. It would help if you also consider taking preventative measures to reduce the risk of these flare-ups.
Also read: Crohn’s Disease and Life Expectancy
Complications Caused by Crohn’s Disease:
- Colorectal cancer: People with IBD have developed an increased risk of developing carcinoma. The abnormal cells form in the lining of the colon or rectum and over time, these cells become cancerous. This is higher in individuals who have had Crohn’s for 8-10 years or more.
- Fistulas: Inflammation from Crohn’s disease can spread across the intestinal wall, forming an abscess. As the abscess increases in size, it creates a small hole in the wall, and this hole can develop into a fistula (an abnormal pathway that connects one organ to another).Sometimes, fistulas form a tunnel from the intestine to the outer surface of the skin called an enterocutaneous fistula (ECF). So many people with ECFs experience at least one complication, such as malnourishment or septicemia (a whole-body inflammatory response to infection). Without treatment, these complications can result in death.
- Intestinal obstruction: is a general complication of Crohn’s disease. An obstruction usually results from a buildup of scar tissue which narrows a section of the colon, making it hard for the stool to pass.
- Perforated colon: Chronic inflammation, abscesses, fistulas, and strictures can weaken the intestinal wall. In the long run, the wall can tear allowing bacteria and other substances to leak from the intestine into the abdomen. The medical term for this is peritonitis. Peritonitis can cause more severe complications, such as blood poisoning and sepsis.
- Toxic megacolon: Toxic megacolon is a very rare yet life-threatening complication of IBD. Although it was said to be more common among people with ulcerative colitis, it also occurs in people with Crohn’s disease. When inflammation causes the colon to expand that it cannot contract, toxic colon is observed. This results in a buildup of gas. This buildup can cause the colon to explode, leaking harmful bacteria and toxins into the bloodstream.
Crohn’s Disease ICD-10 Code:
The 10th Edition of the International Classification of Diseases (ICD-10) is a diagnostic tool, approved by World Health Organization. It is used for clinical communication by providing more information per code and better support for care management, quality measurement, and analytics. This database includes codes for medical diagnosis based on WHO’s a classification of conditions.
The Crohn’s Disease ICD-10 code is K50.90. It can be use to indicate a diagnosis of Crohn’s disease and other medical conditions that have similar symptoms. The code may be applicable to a few Gastroentintestinal conditions such as:
- Crohn’s disease NOS,
- Regional enteritis NOS
The following code(s) above K50.90 contain annotation, and references that may apply to K50.90:
- K00-K95 Diseases of the digestive system
- K50-K52 Noninfective enteritis and colitis
- K50 Crohn’s disease [regional enteritis]
Its approximate synonyms include:
- Arthritis due to Crohn’s disease
- Regional ileocolitis
This is the American ICD-10-CM version of K50.90 – other international versions of ICD-10 K50.90 may be different. Medical professionals and Physicians use the Crohn’s Disease ICD-10 to diagnose the condition which may further help with prognosis and treatment plans.
Crohn’s Disease Diagnosis:

Your doctor cannot diagnose Crohn’s disease on a single test result. They will start with eliminating other possible causes of your Crohn’s disease flare-ups. Several types of tests are make for a diagnosis:
- Blood tests can help your doctor look for potential problems like anemia and inflammation.
- A stool test can help your doctor detect blood in your GI tract.
- Your doctor might ask you to undergo an endoscopy procedure to get a better image of the inside of your upper gastrointestinal tract.
- Your doctor may also request a colonoscopy to examine the large bowel.
- Imaging tests like CT scans and MRI scans are more accurate than an average X-ray. These tests allow your doctor to see specific areas of your tissues and organs.
- Your doctor will likely ask for a tissue sample, or biopsy, taken during an endoscopy or colonoscopy for a closer look at your intestinal tract tissue.
Once your doctor has finished checking all the necessary tests and ruled out possible reasons for your symptoms, they may conclude that you have Crohn’s disease or not.
Your doctor may go on to request these tests several more times to look for affected tissue and determine how the disease is progressing and eliminate the risk of Crohn’s disease fatality.
Management of Crohn’s disease Flare-ups:
Treatment for Crohn’s disease flare-ups varies on the cause of the disease and severity of the condition. The main goal of treatment is to induce remission (the time between symptom flare-ups), maintain remission, and manage any complications of Crohn’s disease over time.
Your physician may recommend one or more of these treatments for Crohn’s disease:
- Corticosteroids: Cortisone, prednisone and other corticosteroids ease inflammation brought on by this autoimmune disease
- Antibiotics: Antibiotics can prevent or treat infections.
- Antidiarrheal medication: Medications like loperamide can stop severe diarrhea.
- Bowel rest: To give your intestines a chance to heal, your doctor might recommend going without food or drink (NPO) for several days or longer. You receive intravenous (parenteral) nutrition or ask to drink only prescribed liquid or have a feeding tube all this time.
- Immunomodulators: They include azathioprine and cyclosporine. These drugs decrease inflammation by suppressing an overactive immune system.
- Surgery: Surgery wouldn’t cure Crohn’s disease, but it can treat complications. You may need to undergo surgery to correct intestinal perforations, blockages, or bleeding.
- Diet: This doesn’t cause it, but it can trigger Crohn’s disease flare-ups. A registered dietician will help you understand how food may affect your symptoms and how a good diet may help you. The dietary changes will help you absorb more nutrients from the food you eat while also limiting any negative side effects food may be causing.
Also read: Crohn’s Disease Self-Care
The Takeaway:
To summarize, Crohn’s is a distressing condition but with treatment, most individuals can enjoy a good and active life. While there is certainly no specific cure for Crohn’s disease, medications and lifestyle changes can keep the infection at bay and prevent complications. There are numerous Crohn’s disease paid clinical trials in Michigan that might have the option to help you and countless others experiencing this disease. Keeping up with your treatment plan, living a healthy lifestyle, and staying away from triggers can help manage this condition.