Last Updated on September 13, 2022
What is Good Clinical Practice In Research?
The Research Industry plays a pivotal role in advancing medicine and improving the quality of life. Research helps to find out answers that are unknown, and assists in filling gaps in knowledge and transforming the way the healthcare industry works. Delivering excellent healthcare services requires meticulous and thorough planning by following the basics of Good Clinical Practice. All of it highly depends on the type of working environment and competency of the workforce of a Clinical Research Organization.
GCP Clinical Research is an ethical and scientific marker for conducting Clinical Trials. Compliance with the GCP (Good Clinical Practice) guidelines ensures that the rights, safety, and well-being of participants are valued and protected. GCP has an integral role in the success of Clinical Research and forms the foundation of Clinical Trials. Having a well-trained competent staff highly endowed with Good Clinical Practices is the key to the success Good Clinical Practice (GCP) Study.
How do the Basics of Good Clinical Practice help in Clinical Trials?
Clinical trials are conducted with sound evidence, meticulous planning, and in compliance with ethical regulations. When conducting clinical research, it is important to take into account the advantages of identifying risk factors as well as to ensure the rights, safety, and well-being of trial participants. It is crucial to obtain subjects’ informed consent and safeguard their confidentiality throughout the basics of Good Clinical Practice (GCP) study.
GCP Clinical Research serves to safeguard the fundamental rights and privacy of trial participants as well as the veracity and authenticity of the data. It also protects the findings that are provided. Clinical Trial supervision duties include choosing study investigators, reporting safety data, and always providing accurate information.
The Regulatory Agency for Human Use promotes a proportionate approach to applying GCP in carrying out clinical research, obtaining participants’ informed consent, and providing staff members with the necessary training.
Basics of Good Clinical Practice GCP Study:
GCP Clinical Research aims to protect the rights, safety, and welfare of participants and annihilate risks, reduce the cost of trials for sponsors as well as participants, and make the clinical trial as seamless as possible for every member involved in it. Abiding in Good Clinical Practices also assures the integrity of clinical data.
Ethical Guidelines in GCP Clinical Research:

GCP Clinical Research aims to create generalizable knowledge that advances human biology knowledge or human health. Clinical research participants enable the preservation of that knowledge. One way to determine their safety or efficacy is by testing new medications or treatments on willing patients.
Clinical research, however, has the potential to take advantage of patient volunteers by putting some people at risk of harm for the benefit of others. The goal of ethical standards is to safeguard both patient volunteers and the scientific method — it is the major element of the Basics of Good Clinical Practice.
Common Ethical Codes that Guide Good Clinical Practice (GCP) Study:
- Nuremberg Code,
- Declaration of Helsinki,
- Belmont Report,
- CIOMS and,
- US Common Rule.
By thoroughly studying these ethical codes, seven principles are proposed to guide the conduct of ethical research:
Social and Clinical Significance:
Research studies are conducted to find out the answers to a particular problem or subject of interest. In the case of the Good Clinical Practice (GCP) Study, the answer should be scientifically valid and valuable enough to justify the participation of subjects and risking their lives for the betterment of a community.
Scientific Facts:
GCP clinical research should be designed in a way that validates the questions asked. The objectives should be clear and understandable.
Fair Subject Selection:
Participants should be chosen in a way that minimizes the risks and adds value to the Good Clinical Practice (GCP) Study. Minorities and people from diverse backgrounds should not be excluded from getting the benefits of a clinical study without a substantial reason.
Risk-Benefit ratio:
It is important to weigh the risks and benefits before conducting GCP Clinical Research as it helps to maintain the safety of the participants.
Independent Review:
Before the commencement of a Clinical Trial, it should be reviewed by a neutral regulatory body. In this case, Institutional Review Board (IRB) reviews all the materials.
Informed Consent:
To keep the research within the ethical parameters, most agree that the participants should make an informed decision regarding participation in the Clinical Trial.
Consideration for Enrolled Participants:
Respecting a participant’s decision to take part in a Clinical Trial is important. They should be valued and respected from the day they enter into the Clinical Trial till the end of the trial. Respecting their privacy and protecting their information, acknowledging their right to change their mind in between the trial, and keeping a check on their well-being during the trial is proof of successful GCP Clinical Research. Most of the monitors take care of these points but are reluctant in sharing the study results with the participants.
Role of ICH-GCP in Good Clinical Practice GCP Study:
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use aims to unify regulatory authorities and pharmaceutical industries to talk through the scientific and technical aspects of pharmaceutical drug development and roster, especially in GCP Clinical Research Trials.
It focuses on improving healthcare to achieve greater conformance by establishing standards in the form of guidelines for pharmaceutical product development and registration.
GCP – Good Clinical Practice Guidelines:
GCP Clinical Research has a defined set of principles that need to be abided by to ensure patient safety and confidentiality. There are 13 principles of Good Clinical Practice (GCP) study. A few of these include:
Compliance with Ethical Guidelines:
Clinical Trials should be carried out in accordance with ethical guidelines to substantiate the results of the trials.
Risk Mitigation:
Before the commencement of a Clinical Trial the risk should be weighed against potential benefits. A trial should be pursued only when there are more benefits than risks. This ensures compliance with the GCP Good Clinical Practice guidelines.
Safety, Well-being, and Rights of Participants:
This principle states that the safety and well-being of a participant are the utmost priority and should be diligently looked upon.
Sufficient Drug Information:
It is essential to have enough information regarding the drug to support the clinical trial. This includes both clinical and non-clinical information about the investigational drug.
Scientifically Rational Protocols:
Focuses on the clarity and precision of a GCP Clinical Practice GCP study.
IRB Review and Adherence to Protocols:
This principle is an important one as it states that all the materials must be approved by IRB (Institutional Review Board) before the commencement of GCP Clinical Research. This is one concept in the GCP (Good Clinical Practice) guidelines.
Inclusion of Qualified Physicians:
For all condition-related queries, a qualified physician or dentist must be consulted.
Who Is Supposed to take GCP Clinical Research Training?

Anyone directly or indirectly involved in a Clinical Trial is required to take GCP clinical research training including research site staff, supporting staff, contractors, and consultants to ensure adherence to the protocols. It must be repeated after every 3 years to assess and refresh the knowledge of all the members involved in the Clinical Trial, according to the GCP Good Clinical Practice guidelines, and to keep them updated in case of any change in the basics of Good Clinical Practice.
Participants of Good Clinical Practice GCP Study:
It is important to understand the roles and responsibilities of participants in GCP Clinical Research. These include:
Regulatory authorities:
Regulatory authorities are responsible for conducting inspections and submitting clinical trial data.
The Sponsor:
The Sponsor is a company or an organization that takes the responsibility for conducting and overseeing a clinical trial.
Monitor:
Monitor is appointed by a sponsor and responsible for looking after the whole clinical trial process.
Investigator:
Investigator is the leading Physician who is responsible for conducting and overseeing the entire clinical trial.
Patients:
Patients are the human subjects participating in the GCP clinical research.
Review Boards:
Review Boards are usually nominated by Institution or if not available then the health body of that country selects one.
Committee:
Committee overseas Sponsors (drug companies).
Clinical Trial Monitoring in GCP Clinical Research:
Monitoring in a clinical trial is a vital part of the Good Clinical Practice GCP study. It ensures:
- Safety and well-being of participants,
- Accurate data from a reliable source, and
- Allegiance to the GCP clinical research protocols.
Selection Criteria of a Monitor in Good Clinical Practice (GCP) Study:
- Monitors should be appointed by Sponsors,
- They should be adequately trained and have sound scientific knowledge, and
- The monitor should have an in-depth knowledge of the investigational drug, protocol, and all the information needed to deliver to the subjects.
What is the Role of a Monitor in GCP Clinical Research?
The monitor in conformity with the Sponsor should make sure that the trials are adequately conducted by following the GCP (Good Clinical Practice) guidelines:
- Acting as a liaison between sponsor and investigator
- Affirm that the monitor has relevant experience and qualification
- Verify the investigational product for its storage time and conditions
- Confirm that the consent form was collected before the trial begun
- Ensure that the investigatory complies with applicable regulatory requirements.
Role Of FDA in Good Clinical Practice (GCP) Study:
FDA modulates clinical studies that are focused on devising proof to support the safety and effectiveness of a medical drug, device, or strategy. All the people involved in GCP Clinical Research are required to comply with the regulations to ensure the safety of human subjects and to maintain the integrity of clinical data.
Institutional Review Board (IRB) in Good Clinical Practice (GCP) Study:
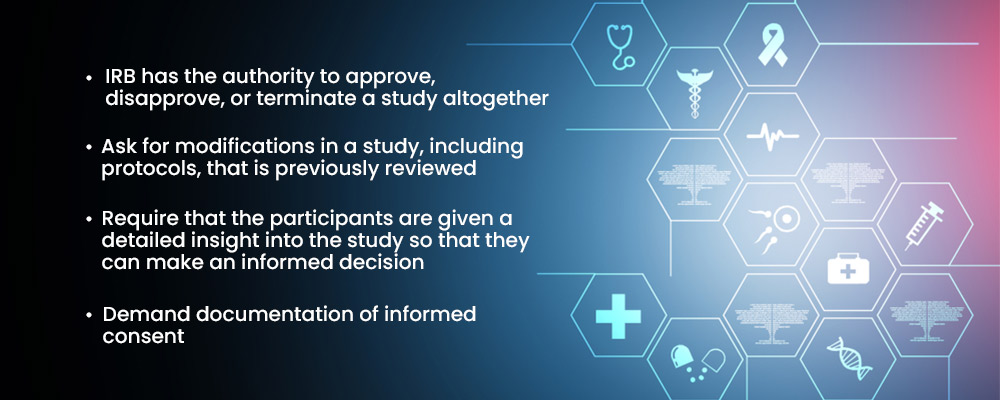
Institutional Review Board (IRB) is a regulatory body that protects the rights and welfare of human research participants. As per the code of Federal Regulation, every study needs to be reviewed and approved by IRB in a Good Clinical Practice GCP Study.
- IRB has the authority to approve, disapprove, or terminate a study altogether
- Ask for modifications in a study, including protocols, that have been previously reviewed
- Require that the participants are given a detailed insight into the study so that they can make an informed decision
- Demand documentation of informed consent
The IRB must have a varied group of members that includes both scientists and non-scientists. At the minimum, IRB must have 5 members to perform and complete the research activities. The members must have diverse backgrounds so that all communities of ethnicities can be included to examine the effectiveness of a drug or a device in a rigorous manner.
Role of Investigator in IRB:
The investigator must:
- Ensure that all the files needed for the IRB to review the proposed research are delivered to it.
- No volunteer should be accepted into a study before the IRB has given it written permission, to begin with, GCP Clinical Research.
- Without the IRB’s previous written approval, make no modifications to the study protocol or deviations from it, unless absolutely necessary to remove urgent risks to participants.
Send a Quick Report to the IRB:
- Modifications or deviations from the protocol, including those intended to protect study subjects from immediate danger.
- Alterations that make participants more at risk or materially modify how the study is carried out.
- Each and every major and unanticipated adverse medication response.
- New drug data could potentially have a negative impact on the study’s operations or participant safety.
How Does Informed Consent Help with Good Clinical Practice GCP Study?
Informed consent and good clinical practice go hand in hand. GCP Clinical Research is a set standard that includes informed consent, as the function of GCP is to protect the participants. Informed consent consists of the 20 ICH-required elements.
Informed consent is a legal document that entails all the information regarding the clinical trial. It involves educating the participants about the risks and benefits of the trial. Informed consent helps the individual to make an informed decision by providing them with all the necessary information regarding the trial to protect them from any harm, as per the GCP Good Clinical Practice guidelines.
A person who willingly consents to participate in a GCP Clinical Research study after being fully educated about it verbally with study staff and after receiving written, signed, and dated documentation is considered to have provided their informed agreement. Throughout the study, a participant’s consent will be repeatedly requested. They will also be informed of any modifications to the study and any other relevant details that might affect their decision to continue participating.
How Does Quality Assurance Play A Role In Good Clinical Practice GCP Study?
Quality Assurance is an integral part of any organization. It is an important element to gauge the quality of a service or a product. Similarly, in the healthcare industry quality assurance has a key role in maintaining the integrity of the subject’s data and ensuring that clean data is delivered to the Sponsors. It allows for conducting planned and systematic actions to make a Clinical Trial a success, in accordance with the GCP Clinical Research guidelines.
Good Documentation and Record Keeping Processes in GCP Clinical Research:
Accurate data documentation and record keeping are indispensable parts of a Good Clinical Practice Study. It shows that the GCP Good Clinical Practice guidelines are kept in mind and followed. There are different ways through which we can ensure good documentation and record keeping in GCP Clinical Research:
- Keep track of all the information and observations relevant to the study. These documents ought to be linked to a specific participant.
- Keep in mind that the information was first recorded in primary materials.
- The veracity of the data is required.
- Any reviewer should be able to reproduce the study using the study documentation.
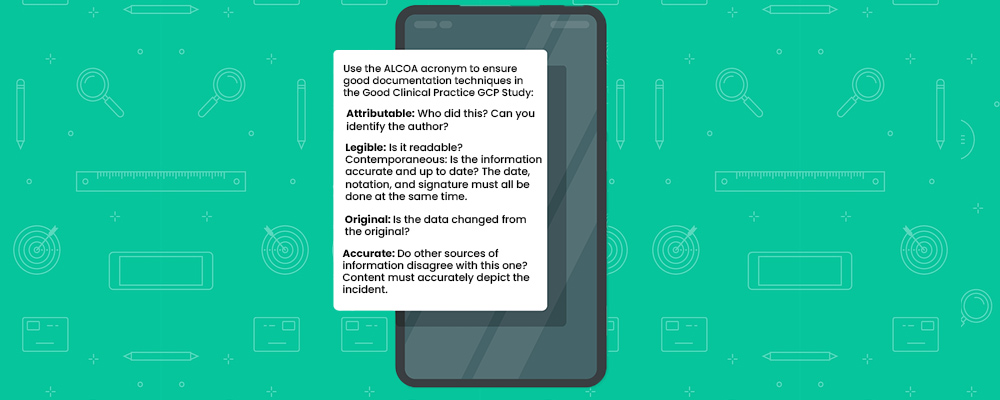
Use the ALCOA acronym to ensure good documentation techniques in the Good Clinical Practice GCP Study:
- Attributable: Who did this? Can you identify the author?
- Legible: Is it readable?
- Contemporaneous: Is the information accurate and up to date? The date, notation, and signature must all be done at the same time.
- Original: Is the data changed from the original?
- Accurate: Do other sources of information disagree with this one? Content must accurately depict the incident.
Significance of Confidentiality and Privacy in GCP Clinical Research:
Confidentiality and Privacy have a major role in the success of a Good Clinical Practice GCP study. They are the cornerstone of ethical and legal guidelines. Protecting the privacy of participants is essential to protect the interests of individuals.
Confidentiality refers to preventing participant data disclosure from the physician’s end to third parties. Ensuring the confidentiality of participants’ data gives the participants the confidence to share their personal and relevant details with the physician that could potentially impact the result of the clinical trial. Breach of confidentiality can be a potential risk in Clinical Research, therefore it is essential to make sure that the staff abides by the GCP (Good Clinical Practice) guidelines that explain the concept of Confidentiality and Privacy.
The Takeaway:
GCP guidelines help to ensure the safety and well-being of participants, which is proof of the success of a Clinical Trial. Therefore, it is essential to perform thorough research, and training and also make the Clinical and Non-Clinical staff involved in the Good Clinical Practice GCP study follow the GCP Good Clinical Practice guidelines.
The significance of the Good Clinical Practice GCP study lies in the questions of why and how the ICH-GCP guidelines came into being. It dates back to the time when the violation of human rights was at its peak. This gave birth to awareness regarding the importance of the need to regulate and control Clinical Trials. This led to the Declaration of Helsinki and The Nuremberg Code, the foundation of present guidelines. Therefore, the ICH-GCP guidelines are contemplated as the bible of Clinical Trials. It holds utmost importance in GCP Clinical Research Study today.
Take a Note:
At Revive Research Institute, all of our Clinical Trials are strictly conducted in accordance with the GCP (Good Clinical Practice) guidelines. All of our research staff including our Principal Investigators, nurses, data operations teams, and everyone involved in the clinical trials are required to train in the basics of Good Clinical Practice and are required to retrain every year to maintain the standards, quality, and integrity of the Clinical Trial as per GCP guidelines.





